Månedens bog
Bog vi anbefaler vores klienter i Nordic Clinic.
Hacks som alle kan bruge til “longevity” som er et hit hele verdenen rundt.
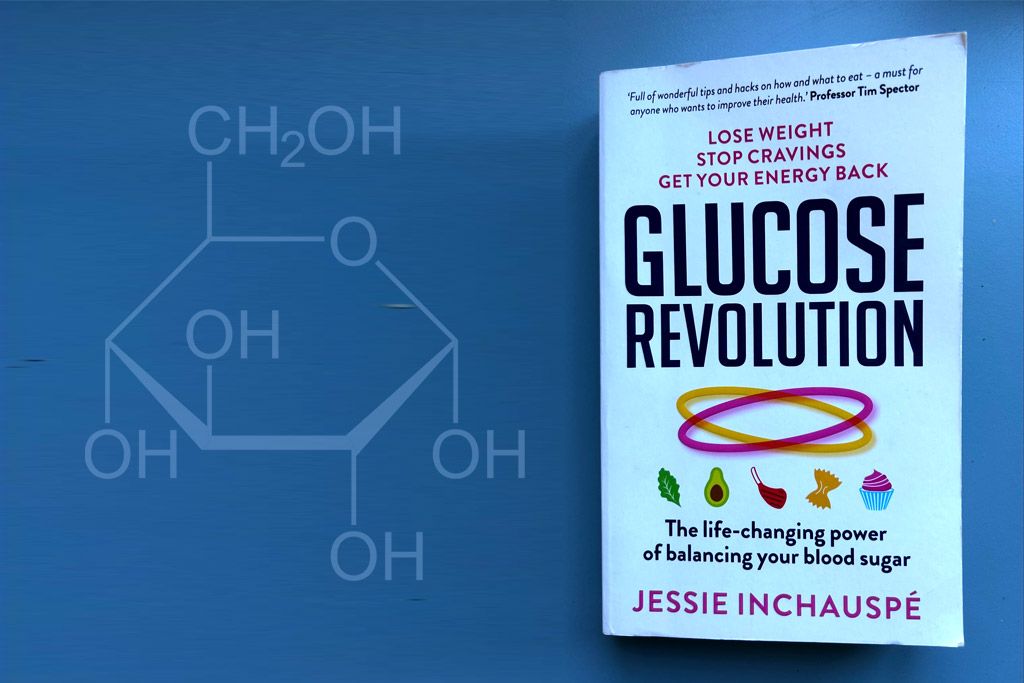
Jessie Inchauspé har skrevet den populære bog: The Glucose Revolution. Du kan google efter den og finde den på mange sprog. Hun er også ret populær på Instagram, da hun viser så fine illustrationer på, hvordan du kan prioritere at spise mad og hvordan rækkefølgen af det du spiser påvirker blodsukkeret. Selvom du er sund og rask, så er det vigtigt at tænke på blodsukkeret alligevel og det kan gøre noget på energi-niveauet og sundheden på dagligt basis. Prøv det selv af. Måske nogle af hendes principper er nemme for dig at indføre.
Vi har selv oplevet vilde blodsukker-rutchebaneture på at drikke matchalatte på havremælk eller bare en gulerodsjuice. Drikke vi tror, er super sunde, og det er de også, men det kræver bare vi husker at drikke dem efter et måltid og ikke alene uden fedt og protein. Vildt at se på en glukose monitor, hvor meget blodsukkeret stiger på havremælk, som er blevet så stort et hit i kaffe-industrien. Vi anbefaler mandelmælk eller kokosmælk, hvis muligt. Det indeholder mindre kulhydrater.
Et langt sundt liv, i fuld vigør
Ønsker du at leve et langt og sundt liv, så kan som sagt enkelte livsstilstiltag gøre en kæmpe forskel for dit helbred. Følger du overvejelserne og principperne herunder kan du ikke blot forebygge livsstilssygdomme som type 2 diabetes, hjerte- karsygdomme og leversygdomme, men måske også opnå sunde celler, hormonel balance, stabilt humør, god energi, perfekt søvn og ikke mindst lav biologiske alder. For ikke at nævne et super sexliv, en uudtømmelig kilde af guldmønter og evig lykke….måske lidt for overdrevet med du forstår hvad vi mener :-). Men du kan med fordel vælge at sætte fokus på at leve dit liv så sundt som muligt, så det bliver så langt som muligt, i forhåbentlig fuld vigør, hvor den kronologiske alder ikke er altafgørende. Tværtimod bliver det din cellulære biologiske alder der spiller en langt større rolle i forhold til din livskvalitet.
Stabilt blodsukker og lavt blodsukker
- Begræns kulhydratindtaget!
Spis mindre mængder eller undgå at spise sukker, ris, pasta, kartofler, brød, og store mængder frugt.Undgå at drikke frugtjuice. - Spis masser af grøntsager (mindst halvdelen af hvad du spiser kan være grøntsager)
- Spis tilstrækkeligt protein – 1 gram pr kg normal legemsvægt
- Spis sundt fedt; smør, kokosolie, olivenolie og hørfrøolie.
- Drik vand, kaffe, the…undgå frugtjuice eller safte-eller sodavand.
Hack dine kulhydrater
Når uheldet er ude, og du kommer til at gøre alt det, du ved ikke er godt for dig (f.eks. spise sukker, kage, brød eller drikke alkohol), så er der nogle ting du kan gøre for at blodsukkeret, på trods, forbliver så stabilt som muligt. Her kommer trylle-tricksne, som ikke virker som en fortrydelsespille, eller tryller problemet helt væk, men blot mindsker skaden der ellers ville ske.
- Spis din mad i denne rækkefølge: Først grønt, så kød/fedt, til sidst stivelse/sødt
Grøntsagerne gør at kulhydraterne fordøjes og absorberes langsomt, så blodsukkeret stiger langsommere og mindre.
- Drik 1 spsk eddike i et glas vand, helst før mad (eller under eller efter, hvis du glemmer før)
Eddiken blokerer de kulhydratspaltende enzymer, kaldet amylase, som gør at kulhydraterne fordøjes og absorberes langsomt, så blodsukkeret stiger langsommere og mindre.
- Spis grøntsager før alt du spiser, gerne med en sukkerfri olie-eddikedressing
Grøntsager sammen med eddike blokerer de kulhydratspaltende enzymer, som gør at kulhydraterne fordøjelse og absorberes langsomt, så blodsukkeret stiger langsommere og mindre.
- Bevæg dig 20 min efter måltidet: gå i 10-20 min eller lav 30-50 squads
Når du har spist, går der ca. 20 minutter før dit blodsukker begynder at stige. Når blodsukkeret stiger, kan du hjælpe med at få det væk fra blodet ved at bruge dine store muskelgrupper.
- Drikker du alkohol, så hold dig til skinny bitch (danskvand, med citron og vodka) og/eller vin.
Øl og drinks indeholder mange kulhydrater. Dertil brug de forskellige hacks herover.
En dag med stabilt blodsukker
Herunder får du indblik i hvordan man kan spise for at opnå stabilt blodsukker. Vær opmærksom på at hvis du har dårlig blodsukkerkontrol kan du måske få det lidt skidt ved blot at kaste dig ud i følgende livsstil. Hav tålmodighed, kast dig ud i det og spis blot færre kulhydrater end du plejer og stille og roligt kan du måske følge principperne herunder
Morgenmad:
- 1-2 spejlæg med ½ avocado og 1 tomat
- Røræg af 2 æg, med masser af frisk babyspinat
- Smoothie på 1 del frosne grøntsager og 1 del frosne bær. Tilsæt 1-2 spsk proteinpulver og 1 spsk hørfrøolie
- Græsk yoghurt (ikke fedtfattig) eller kokosyoghurt med nødder
Frokost:
- Grøn salat med fisk, kylling, kød. Smagt til med usødet olie-eddikedressing
- Omelet med masser af grøntsager (løg, squash, broccoli, tomater)
- Rester fra aftensmad, måske tilsat ekstra grøntsager. Smagt til med usødet olie-eddikedressing
- Varmrøget laks med rucola. Smagt til med usødet olie-eddikedressing
Aftensmad:
- En stor portion grøntsager tilberedt i wok-stil/stir fry, et stykke kød eller fisk stegt på panden eller bagt i ovnen og evt, en håndfuld kartofler eller ris.
- En gryderet med masser af grøntsager, måske med flåede tomater eller lidt kokosmælk, dertil kød, fisk eller rejer og evt, en håndfuld ris eller pasta.
Mellemmåltid:
- 1 håndfuld nødder fx: hasselnødder, mandler.
- Friske gulerødder eller broccoli med hummus
- ½ avocado med en skive cheddarost
- 1 æg med grøntsagsstænger
- Smoothie på 1 del frosne grøntsager og 1 del frosne bær. Tilsæt 1 spsk proteinpulver og 1 tsk hørfrøolie
- Græsk yoghurt (ikke fedtfattig) eller kokosyoghurt med nødder
- Lidt mørk chokolade min. 70% og 5 mandler
Drikkevarer:
- Vand (evt. med bobler, eller citron eller agurkeskiver)
- The/kaffe (hvis med mælk så vælg fløde, sødmælk eller mandelmælk. Hvis det skal sødes så brug stevia, sukrin eller glycin (kosttilskud).
- Ingefærshot uden æblejuice eller anden frugtjuice, blandet op med vand eller danskvand. Hvis du ikke laver det selv, kan ingefærshot fra Økolyst anbefales, da det er uden frugtsukker.
Smagsgivere:
Få gerne maden til at smage af så meget som muligt, hvis du kan lide dette. Brug feks. salt og peber, alle slags krydderier, også krydderiblandinger (uden tilsat sukker), bouillon, fish sauce, eddike, sojasauce, fond eller bone-broth. Hummus eller en lille klat mayonnaise alene, eller med hvidløg eller chilli kan også noget (chilimayo eller aioli).